Community-based health interventions (CBHIs) have been shown to promote health more effectively when tailored to sociocultural aspects linked to health perception, for instance the local language, religion, customs and traditions. Health risk behaviour, for example tobacco smoking, alcohol, unhealthy diet, and physical inactivity, are major global determinants of non-communicable diseases (NCDs). In many Southeast Asian countries, NCDs intervention often take place in the community. By screening for NCDs and promoting healthy behaviour, certain CBHIs aim to reduce health risk behaviours and positively influence solidarity, self-reliance, and social support, which make CBHIs an effective way to modify behavioural change and increase the prevention, management and care of NCDs.
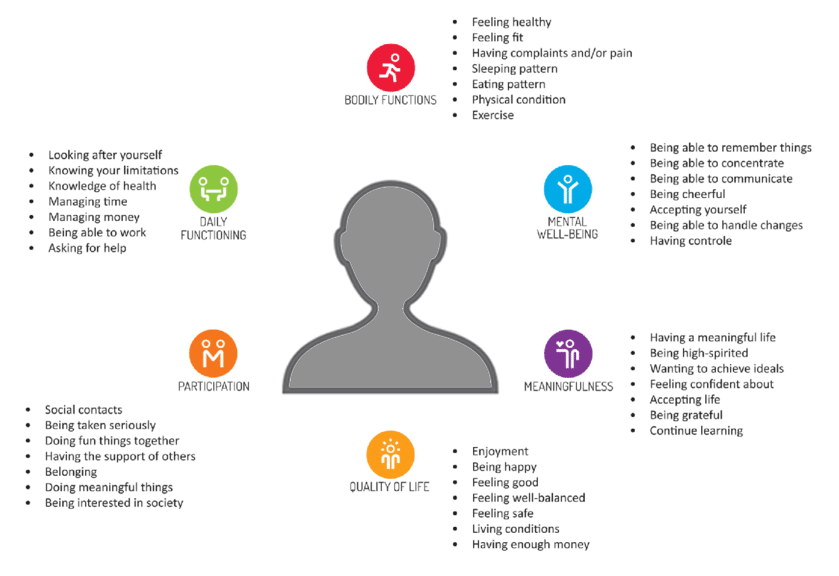
Contextual conditions highly influence the way people perceive their health, and health perception is strongly associated with health behaviours and outcomes. Therefore, it is important to adapt CBHIs to sociocultural needs. The ‘Concept of Positive Health’ introduced by Huber (2011) addressed a person’ health needs in six major dimensions: bodily functions, mental wellbeing, meaningfulness, participation, daily functioning, and quality of life (see above figure).
These dimensions address health in a dynamic and comprehensive way. According to this concept, health is influenced and affected by a person’s social environment, real-life situation, involvement in society and spirituality. With this broader definition, health is not merely the absence of a disease or infirmity, rather it is recognised that health is established and influenced by, to a great extent, a persons’ health perception, in turn associated with the cultural and contextual environment in which they live. Incorporating the dimensions of positive health can guide the adaptation of CBHIs to fit the context, thus more effectively inducing the promotion, prevention and management of health.
Contextual adaptation of CBHIs is dynamic, and to date there is no scientific base or practical guideline on how to do this. The development of a ‘cultural and contextualisation guideline’ with checklists to support the adaptation of the CBHIs to the local setting, may help to increase effectiveness. To address this gap the study aimed to develop checklists to support contextual adaption of community-based health interventions based on the concept of ‘Positive Health,’ and produce a user guideline for implementation of these checklists.
For this research, we used a Participatory Action Research (PAR) approach which has two distinguishing characteristics: the participation of stakeholders as partners in the research process and a commitment to action for social change. In every phase of this research we consulted with various groups of stakeholders to elicit local and globally perspectives on CHBIs, to deepen and enrich the contextual aspects of ‘Positive Health’ We worked in collaboration with academia, local and international NGOs and universities and health policy makers in the project countries, and with NGOs based in various regions of the world. During the first phase, a theoretical framework and focus were established, and a first group of stakeholders were consulted. In the second phase, based on the findings from the first phase the checklists were drafted and a guideline for application of the checklists was developed The guideline was then tested and evaluated with the second group of stakeholders. In the third phase consultations were conducted with stakeholders based in various regions of the world. In the last phase, all data will be synthesised and the final guideline will be formulated.
Written by: Zinzi Pardoel,University Medical Centre Groningen